The Full Psychiatric Assessment – Seeing the Whole Person
Case 1 - Episode 3
“I’m just trying to hold it together. But I don’t know how much longer I can.”
In Episode 2, we built a structured, empathic HPI[1] that helped us understand when Sarah’s symptoms started, what triggered them, and how they’re affecting her life.
Now it’s time to zoom out.
Because no matter how compelling the symptom story, it exists within a wider human context.
And our job is to see the whole person.
Why the Full Psychiatric Assessment Matters
Too often, we rush from symptom to diagnosis.
But real psychiatric healing depends on meaning, function, and context.
The full psychiatric assessment[2] answers questions like:
Who is this person developmentally and culturally?
What traumas or life patterns shaped their current struggles?
Are they safe, stable, supported?
What are they trying to communicate—through symptom, silence, or survival strategies?
Let’s walk through the key domains of a full assessment[3], using Sarah as our guide.
Biological Assessment: What’s Happening in the Body and Brain?
Key Questions to Ask:
Any family history of psychiatric illness or suicide?
Past medical or neurological issues?
History of head trauma, seizures, or other relevant conditions?
Current medications, including supplements or over-the-counter use?
Any substance use, including caffeine, cannabis, alcohol, or stimulants?
Sarah’s Story:
Father has a history of “meltdowns” and was hospitalized once in his twenties.
No medical issues or past surgeries.
Taking Adderall occasionally (not prescribed), large amounts of caffeine, no alcohol or cannabis use reported.
No menstrual irregularities, no disordered eating, sleeps ~3 hours/night.
Clinical Implications:
Consider stimulant-induced psychosis, especially with sleep deprivation.
Watch for genetic loading—possible bipolar or schizophrenia spectrum.
Need to rule out thyroid, B12, substance-induced states.
Psychological Assessment: How Does She Experience Herself and the World?
Key Areas to Explore:
Cognitive function: memory, attention, abstract thinking
Mood and affect congruence, range, reactivity
Thought process and content: paranoia, delusions, thought insertion
Insight and judgment: can she reflect on her condition?
Defense mechanisms: projection? denial? minimization?
Sarah’s Presentation:
Tangential but not disorganized speech
Paranoid content, possibly persecutory delusions
Flat affect but tearful at moments
Insight: limited but not absent (“I know something’s off”)
Judgment: impaired (Adderall misuse, isolation)
Social & Cultural Assessment: Where Is She in Her Life Story?
Questions to Ask:
Who are your supports?
What was your childhood like?
Are there any cultural or spiritual beliefs that influence how you understand this?
Are you experiencing discrimination, financial strain, or housing insecurity?
Sarah’s Reality:
First-generation college student
Estranged from her father, close to her grandmother
Grew up in a household where mental illness was “a weakness”
Recently moved off campus due to financial pressures
Feels “out of place” and disconnected
Developmental Assessment: What Stage Is She Navigating?
Using Erikson’s psychosocial stages[4], Sarah is navigating Identity vs. Role Confusion (ages 12–24).
“I don’t know who I am anymore. I used to be the smart one. Now I’m the girl who hides in her room.”
Psychosis or severe mood symptoms during this developmental stage can derail identity formation. Our task is not just to reduce symptoms, but to support the rebuilding of a coherent self.
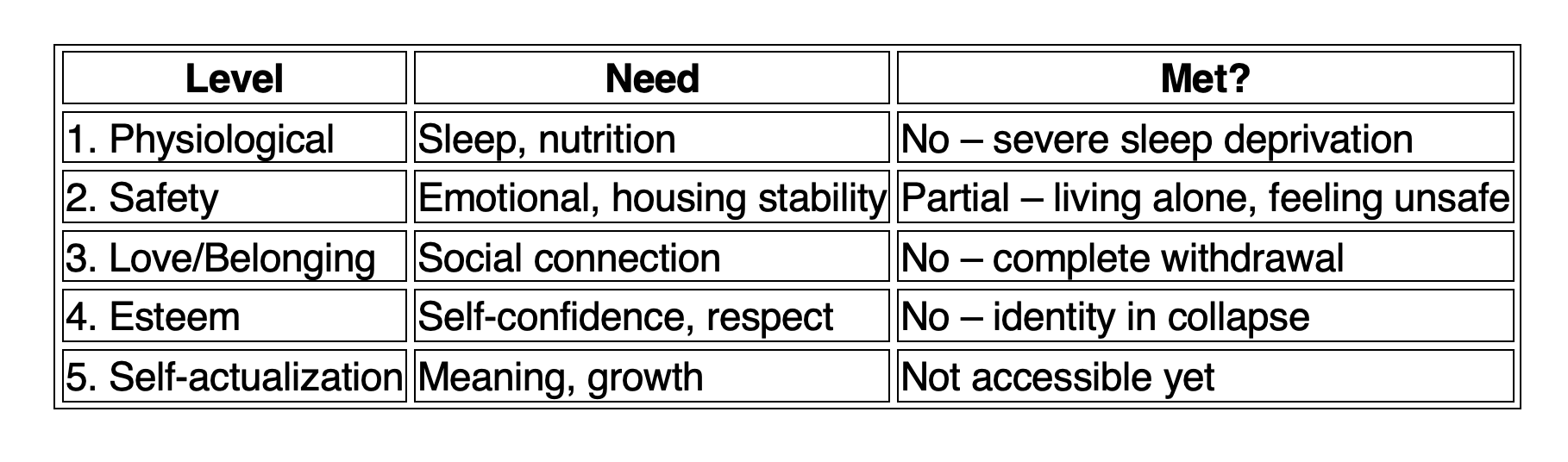
Needs-Based & Maslow-Informed Formulation: What’s Most Urgent?
Let’s look at Sarah through Maslow’s hierarchy:
Implication:
Before we talk medication or therapy, we must restore basic safety and connection.
Sleep. Nutrition. Warmth. Emotional containment.
Psychiatry is not just neurochemistry. It is human need in crisis.
Putting It Together: The Formulation So Far
Sarah is a 22-year-old college student presenting with acute-onset paranoia, auditory hallucinations, and functional decline. Her symptoms appear to be precipitated by stress, isolation, stimulant use, and sleep deprivation. Her developmental stage (identity formation) is disrupted, and she has unmet physiological and safety needs. Insight is partial. Cultural stigma may limit help-seeking. Family history raises the possibility of a mood or psychotic disorder.
This is not a diagnosis.
This is a formulation—our interpretive bridge between data and diagnosis.
Coming Up Next: Episode 4 – Differential Diagnosis & Clinical Reasoning
In the next episode, we’ll explore:
How to organize differentials (psychosis vs. bipolar vs. substance-induced vs. trauma-related)
What to look for to rule in or rule out each one
Which labs, assessments, and collateral data to gather
And how to avoid diagnostic anchoring too early
Reflective Prompt for You
Think of a case where a patient’s unmet needs, not just symptoms, were the key to healing.
What did you notice? What shifted when you addressed the human before the diagnosis?
Share your thoughts—and stay tuned for the next episode.
Would you like to be part of a growing community of exceptional psychiatric nurse practitioners on LinkedIn? If so, click here to join our SWEET Psych NP LinkedIn page.
References:
[1] Adler, Herhert M. "The history of the present illness as treatment: who's listening, and why does it matter?." The Journal of the American Board of Family Practice 10.1 (1997): 28-35.
[2] Gomez, María Fernanda, and Mary Alice O’Dowd. "Psychiatric assessment." Psychiatric Aspects of HIV/AIDS. Philadelphia: Lippincott Williams & Wilkins (2006): 39-47.
[3] Andrasik, Frank, Jeffrey L. Goodie, and Alan L. Peterson, eds. Biopsychosocial assessment in clinical health psychology. Guilford Publications, 2015.
[4] Darling-Fisher, Cynthia S. "Application of the modified Erikson psychosocial stage inventory: 25 years in review." Western Journal of Nursing Research 41.3 (2019): 431-458.
Would you like to be part of a growing community of exceptional psychiatric nurse practitioners on LinkedIn? If so, click here to join our SWEET Psych NP LinkedIn page.